Emergency medical service workers in America face a daunting winter. The number of COVID-19 cases is surging as is the number of deaths caused by the virus. The expectation is that after the holidays the numbers will rise higher as people come together to celebrate despite warnings from medical professionals to stay apart.
According to a recent report from EMS1 that analyzed data available as of September, EMS workers appeared to have the highest mortality rate of all health care workers fighting the coronavirus. While the numbers are few and primarily from New York City, the report extrapolated that frontline EMS providers were dying at a rate of 91 per 100,000 persons.
Maine’s frontline EMS workers have fared relatively better, but the threat remains.
“We are always on edge, because we don’t know what the next call is going to bring,” Blaine Bacon, paramedic and Delta Ambulance chaplain, said recently. “We’re going out into the field that is already inherently, if you will, dangerous.”
Up to now EMS workers have relied on the standard litany of prevention: wear masks and personal protective equipment, deep clean vehicles and equipment used on the job, wash your hands, keep your distance to assess a patient. But eventually the job becomes hands-on.
Now they have one more defense: the vaccine, a game-changer which, as Delta paramedic Corie McCarthy puts it, becomes “part of the game” that living with the virus for a long time will become.
Exposure to COVID-19 for EMS workers comes in the least expected situations.
Nathaniel Lombardi and partner Rebecca Quinn were exposed to the virus on a routine call in which there was no indication that COVID-19 was present.
“It was a 911 call in Oakland, and the guy had weakness from anemia,” said Lombardi, an advanced emergency medical technician with Delta. “Two weeks before he had a blood transfusion.
“We transported him to Augusta, and he was admitted and tested and it came back positive. Two days later we received an email from Maine EMS saying that you had been exposed by someone who was either positive or pending positive results. Which doesn’t tell us anything.

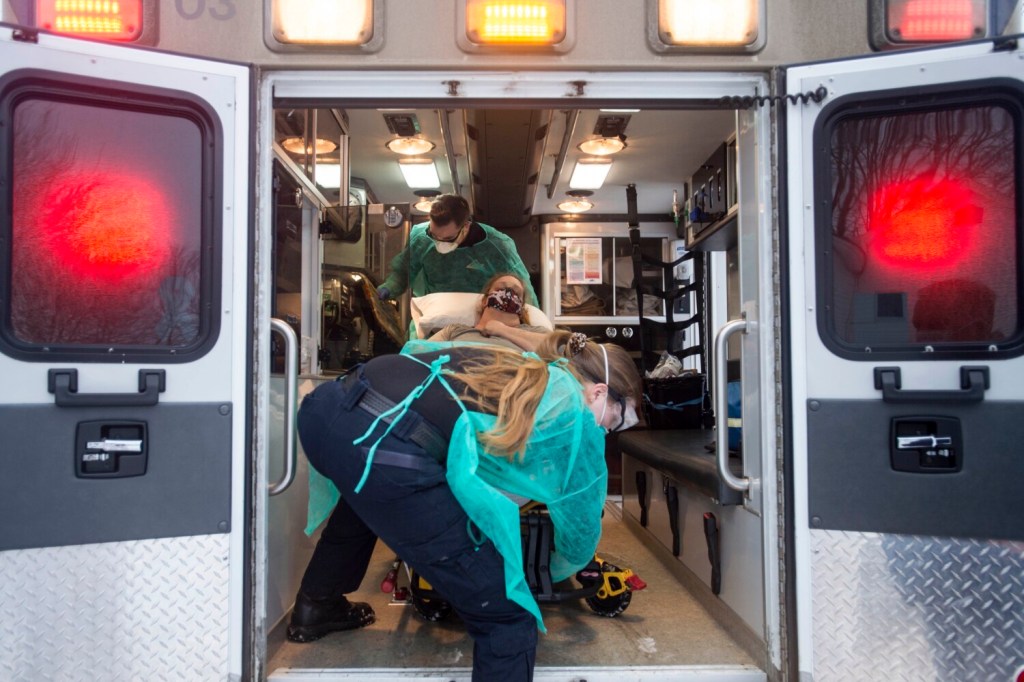
Nathaniel Lombardi, an advanced EMT, assists an elderly woman to the ambulance Dec. 21 in Fairfield. Michael G. Seamans/Morning Sentinel
“There was nothing at all that looked like COVID. No cough, no fever, no symptoms,” Lombardi said.
The virus can be hidden just long enough to catch a person unprotected. Two Delta paramedics were exposed to COVID-19 during a recent transfer.
A patient was flown by plane from a hospital in Maryland to Togus. The patient was asymptomatic. Flight nurses were informed that the patient tested negative. Upon the patient’s arrival at Togus, another test was administered but with a positive result and after exposing an ambulance crew and flight crew to the virus.
“And that’s why this disease is so insidious,” said McCarthy.
Frontline health care workers, such as those providing emergency medical services, have more variables in play when it comes to personal safety. Unlike hospitals, which have designated units for COVID-19 patients, paramedics and EMTs are entering the homes of people who are too sick or don’t have the means to get to a hospital.
They initially assess a patient from 6 feet, but then treatment of patients in their homes becomes hands-on as is preparing to move them. More treatment is administered on the way to the nearest hospital, which in rural Maine can amount to hours. The time of exposure to a person who is possibly high risk can be significant.
“So, what was, if you will, on a scale of 1-10, what was a dangerous situation at 5 normally without COVID,” Bacon said. “Now that we’re (more than) 6 months into it and into the Christmas season, that has been ratcheted up to a 6 or 8, and we have to keep that in mind.”
The Moderna vaccine that was recently approved is in the process of being distributed to frontline EMS professionals, paramedics, EMTs and other staff.
“It’s one more layer of PPE at my disposal,” McCarthy said. “I was not going to do it because I have faith in my immune system, but I have elderly parents with multiple comorbidities. If they get sick, they’re my responsibility.”
Paramedic Michael Record, 37, received the vaccine Dec. 23. “I think it has helped. It makes me feel better,” he said.
Like McCarthy, he sees the vaccine he has received as a way of protecting patients. “There’s always the unintended fear that we are going to infect a patient.”
Joe Brichetto, paramedic intern at Delta Ambulance, sees the vaccine from a different perspective. “If you want to be a progressive provider, you believe in evidence-based science. Taking the vaccine shows faith in the science.”
Send questions/comments to the editors.